This year marks the 500th anniversary of the birth of anatomist Andreas Vesalius. Born in 1514 in modern-day Brussels, he was educated in France before taking up a position teaching surgery and anatomy at the University of Padua in Italy.
At the time, knowledge of the human body was based on the study of classical texts rather than empirical observations and medical practice relied heavily on the writings of the Greco-Roman physician Galen. Understandings of anatomy were limited, despite the rising interest in human sciences and popularity of naturalistic illustrations in the 16th century. Furthermore, many assumptions were inaccurate as they were based upon findings made in the dissection of animals such as monkeys and dogs.
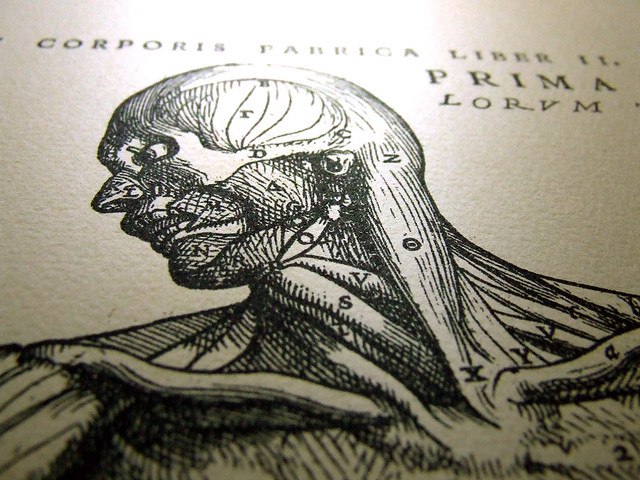
Unlike many of his colleagues, Vesalius rejected this theoretical approach to medicine. Instead he taught anatomy through personal demonstrations and the dissection of human cadavers. From 1538 he began to publish anatomical illustrations and in 1543 released his famous work De Humani Corporis Fabrica (On the Fabric of the Human Body). This ground breaking book contained over 600 woodblock engravings and its 7 volumes detailed the skeleton, muscles, vascular system, nerves, abdomen, thorax and brain. While it was not the first time that the human body had been shown after autopsy the intricacy of the illustrations meant that it was the most accurate anatomy text to date. It disproved many of Galen’s theories and the integration of images with textual descriptions was considered highly innovative at the time.
Through his teaching and publications Vesalius revolutionised the study of anatomy by demonstrating the importance of first-hand observation for medical training and scientific discovery. De Humani Corporis Fabrica thus represents a radical change in the way anatomy was approached by promoting dissection as the most scientific way of studying form and function. Anyone who has seen images from the book will no doubt agree that it is also a work of great artistic value as it depicts bodies in dynamic poses against beautiful classical backgrounds.
Vesalius later left teaching to work as the imperial physician for Emperor Charles V. He continued to perform dissections and publish on anatomy until his death in 1564.
Image credit
R. C., C. (2005). Vesalius [Image]. Retrieved from https://www.flickr.com/photos/celesterc/415837587
References
Dominiczak, M. H. (2013). Andreas Vesalius: his science, teaching, and exceptional books. Clinical Chemistry, 59(11), 1687-1589.
Kemp, M. (1998). Vesalius’s veracity: implications of illustrations of surgical tools and anatomy by Andreas Vesalius. Nature, 393(6684), 421.